There is a lot of talk about pandemic preparedness, but what does it mean? Too often there are narrow, medicalised versions – focused for example on drug stockpiling, vaccine banks and so on. This Covid Collective report – Pandemic Preparedness for the Real World – has critiqued this view, offering a wider perspective on pandemic preparedness. What might a more locally rooted version of pandemic preparedness look like? Can wider understandings of how building resilience within communities can assist? There have been many important lessons emerging from the pandemic experience, but are they being learned? The relatively quiet and calm inter-pandemic period is crucial, as there will surely be a next one.
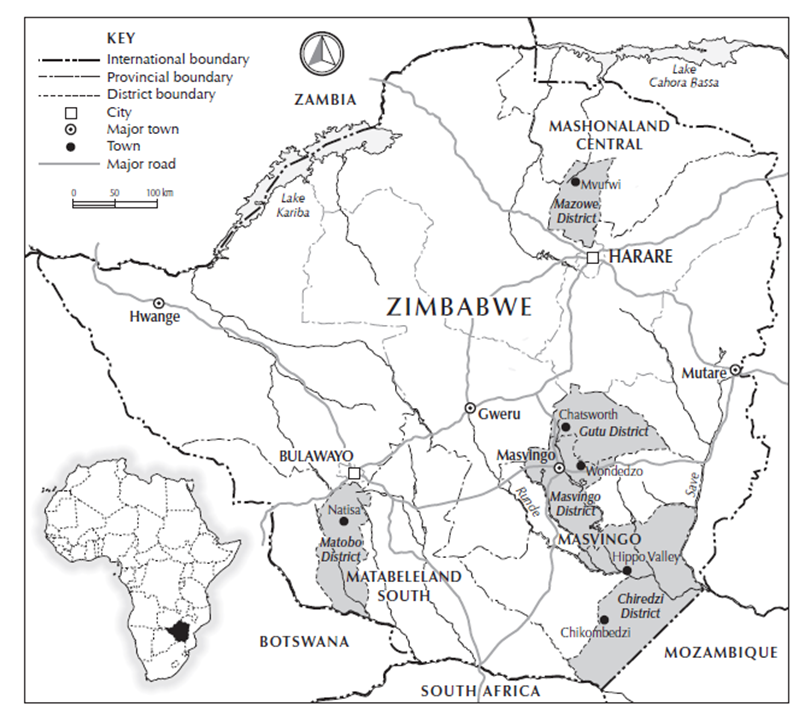
During November and December 2022, we tested the ideas in the Covid Collective report with different communities in six sites across Zimbabwe in a series of dialogues. This built on real-time research in the same settings from March 2020 to February 2022. From Chikombedzi in the dry, far south, via the sugar estates of Hippo Valley and Triangle to the livestock farming area of Matobo and the maize/horticulture zone of Masvingo and Gutu to the tobacco growing area of Mvurwi, we engaged with a real diversity of rural settings (see map). There has been remarkably little commentary or research on rural contexts and we aimed to fill this gap. Our work did not rely on snapshot surveys, but on real-time discussion and reflection – involving six field researchers living in the sites, a field coordinator and Ian Scoones at IDS.
The result was a series of 20 blogs published from March 2020, when the first case identified in Zimbabwe, to February 2022. They are all available on Zimbabweland, and also in a new book, which can purchased or downloaded online.
About 20 people who had engaged with our real-time learning during the pandemic were invited to the dialogues, each of which lasted around 3 hours, with discussions following on over lunch. Participants included farmers, local leaders, church leaders and government personnel. In one dialogue we had representatives from five ministries: Agriculture (Agritex), Health (a nurse and village health worker), education (teacher), local government (a councillor) and Home Affairs (police), along with farmers and others. We invited participants to reflect on lessons learned during the COVID-19 pandemic and the implications for preparing for a next pandemic.
Following the wider COVID Collective report, we discussed three themes: the diverse forms of knowledge, the role of reliability professionals and how formal and informal institutions interact. These combined to generate an understanding about how resilience – and so preparedness – can be built.

Knowledge
A key theme from our real-time reflections and from the dialogues was the importance of making use of multiple knowledges. Under conditions of uncertainty, using varied, plural knowledges is essential, people argued.
In one of the dialogues there was an interesting exchange around how local knowledge about treatments (which became really essential during the pandemic) was devalued by formal medical knowledge systems. A particular concern was vaccines, around which there many concerns expressed. Were these being used to experiment on or worse exterminate Africans? What was the role of the Chinese in this? This raised in particular the whole question of trust in knowledge and how it carries authority – and particularly trust in the state. This was clearly lacking for much of the pandemic and remains a big challenge for preparedness plans.
During the pandemic people felt very much on their own, without the help of the state, but the processes of local innovation and information sharing were impressive. The huge array of local remedies – centred of course on the famous plant Zumbani – became central to how people managed the disease. These were shared rapidly through WhatsApp groups, allowing knowledge for example of the Omicron variant to spread from our sites in Chikombedzi near the SA border to Mvurwi and on to the UK within a week or so – far, far faster than the published scientific information and public health advice.

So, what are the implications for pandemic preparedness. The dialogues confirmed that it is vital that different knowledge systems work together – not just informally but formally. This means more investment in assessing local treatments and integrating them into pandemic responses. Also important is the task of reinforcing the knowledge networks that allow the exchange of validated information (not just from public health sources) across communities and into the diaspora. And all of this exchange must help build trust between different sources of expertise, avoiding the dangers of vaccine anxiety for example experienced this time.
Reliability professionals
When health systems are weak and ineffective in the face of an unknown threat, then certain key professionals on the front line, embedded in networks become key. This is an important lesson from Zimbabwe. Literatures on critical infrastructures (for example water or electricity supply systems) tell us that it is ‘reliability professionals’ – not standardised protocols and routines – allow for the services to be delivered, even in contexts of high input variability. They can scan the horizon for impending dangers, while attending to day-to-day responses on the ground.
Who were these reliability professionals during the pandemic? In our real-time research we met one – a young nurse at a rural hospital. He had been training at the very beginning of the pandemic in a large hospital in Harare and had learned some of the features of COVID-19. His superiors in the hospital were fearful as they knew that COVID was coming – particularly given the proximity to the South African border. The Ministry had cut and pasted some instructions from WHO – it was all they had – but these were not enough.
When the first disease arrived in the area (during the delta phase), he worked with other local officials – traditional leaders, church pastors, heads of women’s groups – to share information but also learn from the ground. He had a good idea of the big picture, but also a sense of what was happening locally. As the pandemic changed (as it soon did), then he instituted new arrangements at the hospital and helped patients in the wards and at home. He was allowed to do this by his superiors, but it wasn’t in his job description. Crucially, he was given the latitude to use his professional skills and his networks to generate reliability in a difficult setting. But this work was not recognised or rewarded.

There are always people like him. In one of our dialogues, we heard of a Village Health Worker and an Environmental Health Technicians, who played similar roles. But it could equally have been a church leader, a party official, a councillor or whoever. The important point is that to generate reliability in the face of uncertainty –and so assured preparedness – you need these people, and their networks. And they need to be rewarded and recognised.
Institutions
There was some quite heated debate in our dialogues about the role of formal institutions in the pandemic. As in our real-time reflections, there was much critique of heavy-handed, unthinking approaches to lockdowns. Everyone appreciated why COVID was a disease of crowds, but did not understand why this meant livelihoods being undermined through lack of transport, closed markets and so on and the education and mental health of children compromised through closed schools, leading to wider social problems of drug taking, teenage pregnancies and crime?
Many thought it was these lockdown measures that caused more hardship than the disease itself. Why couldn’t the Ministry of Health relax the form of lockdown over time as the disease changed with different variants? Why couldn’t the police allow for certain types of marketing (say door to door not large market gatherings)? Why couldn’t the education ministry allow classes to be held in smaller groups for shorter periods, so kids at least had something to do? Why couldn’t the police allow some church services if they were safe, without large crowds? Why couldn’t the ministries speak with each other, so people could make the case that lockdowns were causing untold hardship.?
We always talk about cross-sectoral coordination and integration, but the tendency to centralise and control is strong, especially in an emergency. However, such interaction does happen at the local level (all the people from the five different ministries at one of our dialogues knew each other – but they rarely met together). The problem is that decentralised decision-making is often restricted from on high. The opportunities to negotiate compromises at the local level was because the lockdowns were national requirements (often simply replicating global advice) and implemented with a military style, top-down approach. But global even national advice may not make sense – a pandemic is always local and the politics of response must be local too.

So, a key lesson for preparedness is to decentralise, to trust local negotiations and to be flexible in implementation, responding to local conditions. This may help (in part) address the lack of trust people had in formal institutions because of the nature of an often predatory, autocratic state. In our real-time discussions there was no love lost between farmers and the police who were endlessly taking bribes, preventing marketing and so on. But interestingly in our dialogues, after some barbed exchanges, there developed more of a compromise; an acknowledgement that during the pandemic the police were following orders, working absurdly long hours and were barely paid. Talking together and building relationships helps institutions function better. This work is vital for being prepared for the next pandemic.
Rural people in all our sites have a good understanding of the epidemiology, which improved impressively through the pandemic (often again rather faster than the science). But they also knew how their livelihoods had suffered. Making sure that pandemic responses are livelihood-compatible – perhaps working out a series of options – is vital, and public health and livelihoods more generally must be seen in one holistic approach with local people and formal institutions working together.
Resilience
These three themes together offer insights into how to build resilience in ways that allow people to be prepared for the next pandemic. There is a lot of lip service paid towards ideas of community resilience in the health sector. Indeed, resilience is a development buzzword that often lacks meaning, even if it attracts donor dollars (see our BMJ-GH paper for a reflection).
So, from our studies what is resilience? First, resilience isn’t a thing that can be planted, implemented, created as part of a project, it’s a process, emerging from relationships. Second, resilience isn’t just about bouncing back to what existed before (often vulnerability and poverty), but it’s about transforming structural relations – yes, it’s political. Third, building resilience at community level is essential, but it’s not a panacea, or an excuse not to build the staff, stuff, space and social support central to health systems, as Paul Farmer liked to put.
The ‘communities’ in our research sites are not uniform – contests exist between those with different religious beliefs, between men and women, young and old, rich and poor. Finding a collective way through the pandemic was always negotiated politically, and some were left behind. As with all pandemics, COVID-19 accentuated already existing inequalities and vulnerabilities – meaning that local solutions through romantic visions of community action were not enough and external intervention and support was needed.

What emerged through our discussions was the understanding that the resilience building was all about relationships. The work of reliability professionals focused on relationships and networks (even if centred on a skilled individual), while debates about knowledge were about how different knowledge systems need to relate. Equally, innovation for a more resilient outcome had to involve multiple actors interacting with each other. And, in relation to institutions, again it was all about working together, between ministries and between the state and local actors, with different interests.
In other words, while focusing on the community (broadly understood, and often stretching far through knowledge networks), community resilience should not result in a reification of indigenous knowledge or local ‘community’ practice, somehow isolated from the world. Instead it involved diverse communities interacting with a range of players, including the formal health system. In other words, a hybrid, plural health system was envisaged as the basis for long-term resilience, and the cornerstone of pandemic preparedness.
Lessons and priorities
Where does all this leave us? How has learning in a pandemic and convening dialogues about it afterwards help us develop more effective approaches to pandemic preparedness?
We need to do better than last time. Those countries that were according to WHO the most prepared for a pandemic, had some of the worst outcomes (including the UK and the US). Why was this? It was because they relied on a narrow form of preparedness, reliant on a particular type of knowledge (mostly epidemiological modelling) and a standardised approach to pandemic response (movement control, lockdowns etc.). What they didn’t do was listen to local reliability professionals in decentralised institutions (the doctors and nurses and local government workers in the British Asian communities in the UK Midlands, for example). Nor did they work with the most vulnerable communities (in the case of the UK/US, densely packed multigenerational urban households) to help build resilience (of networks and relationships).
The four themes that emerged from Zimbabwe are therefore as relevant in the UK or the US. But they need to be thought about and implemented in different ways, with local contexts in mind. This is the job now – in the inter-pandemic period when things are calmer and lessons still fresh in the mind. It’s too easy to forget and go for knee jerk responses that replicate past mistakes when a new emergency arises. The impulse to centralise through a securitised, authoritarian response is strong, but other alternatives are essential and need to be fostered now.

Three priorities to help build resilience for preparedness emerge:
- Support knowledge networks that connect formal and informal, local and scientific knowledges, and carry out research on local treatments and the processes by which they are developed and shared.
- Identify and map reliability professionals and their networks across communities, and provide support and recognition to them
- Encourage the decentralisation of decision-making across ministries, including convening cross-sectoral fora for emergency pandemic response.
All of these priorities need to be addressed now. There’s an important role for donors in this, including providing contingency funds at the local level to allow for rapid response around knowledge sharing, reliability professional support and decentralised institutional interaction.
Virtually none of these things are being done in Zimbabwe yet (or indeed anywhere else), and it will require significant finance both to local communities and the state in ways that are flexible and crucially with finance arriving in advance of the inevitable next crisis.